—–
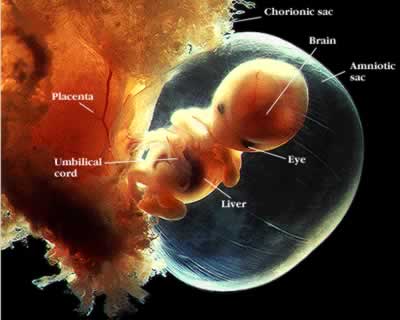
Part of the training to become a Family Medicine physician requires the Resident to have the ability to successfully assist a woman in the delivery her child. Depending on your religion, culture, and/or understanding of human biology, when the baby exits the vaginal canal and lets out its first cry, its life has begun.
Being a part of this experience has led Family Medicine to adopt a credo of “from the cradle to the grave”, as we have the unique blessing to care for patients from the beginning of life until death becomes us.
Nearing the end of my Intern year as a Family Medicine physician, I have now had the opportunity to train as a physician on the Obstetrics and Gynecology (OB/Gyn) service two times. The first four weeks occurred in the first half of my year and were a whirlwind of stress and re-introduction to a field of medicine which I had barely survived as a student.
—–
—–
During those four weeks, I constantly found myself on edge, not only because of my experiences as a student, but because I found myself as the least seasoned member of a team responsible for making sure each and every baby let out its first cry.
While a sense of relief and pride would wash over me when each baby boy or girl let out its first little squeal, most often while I was still holding it in my gloved hands, I was still tasked with several steps to assess the health of the mother after handing off the baby to the pediatrician who stood awaiting my delivery.
—–
—–
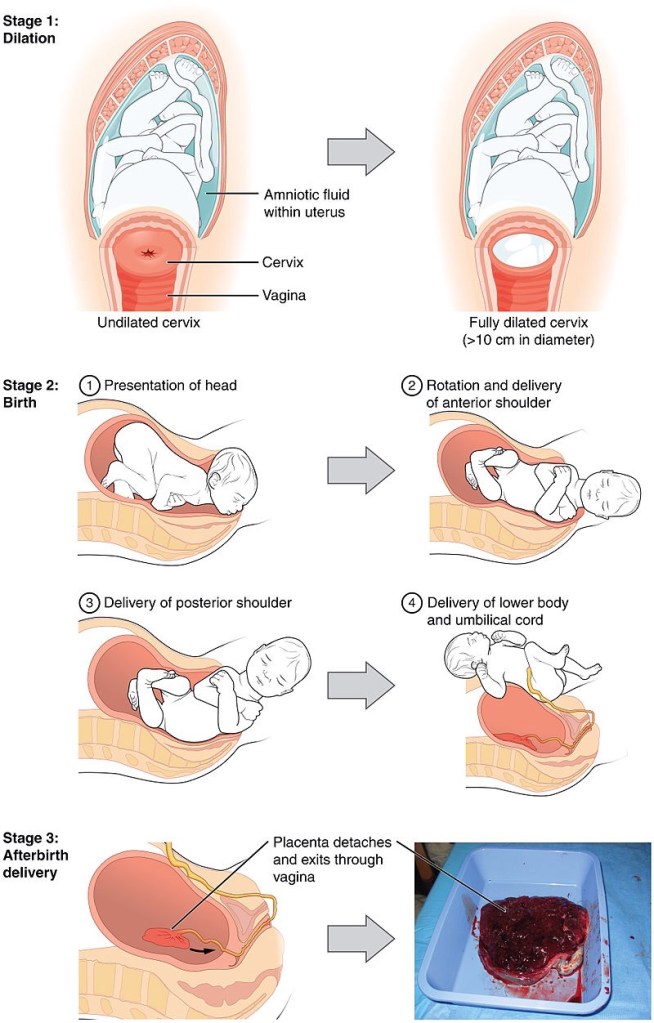
Those additional steps were the cumbersome parts I would rehearse in my head while staring intently at the woman’s vagina as I used my fingers to create the space needed to assist the baby’s head from tearing perineal tissue. Often times, my mind would go blank as soon as the baby made its way into my arms.
After what seemed like an eternity, which properly calculated only totaled 4-5 seconds, I would begin assessing the mother’s health, including any vaginal lacerations which may need repair, massaging the fundus of her uterus to determine the likelihood of a postpartum hemorrhage, and carefully tugging at the umbilical cord still attached to the indwelling placenta.
—–
—–
Typically within 10 minutes I would have transitioned from the foot of the bed, having delivered the newborn and the placenta, as well as completing the necessary postpartum assessments, to clickety-clacking away at the computer to document the successful delivery.
—–
—–
My second go-around on the OB/Gyn service was nearly identical in substance to the first four weeks: women of different stages of pregnancy coming into Labor and Delivery Triage to be told if they were or were not in labor, often requiring me to perform speculum checks and cervical exams; actively laboring women begging for epidurals and anxiously awaiting their newborn while I paid hawk-like attention to the monitors assessing fetal heart tones and uterine contractions; rounding before the crack-of-dawn on women post-delivery, assessing their postpartum needs; and imparting my seemingly minimal medical and clinical knowledge of Obstetrics and Gynecology to the even less-knowledgeable medical students I was tasked with teaching.
But while the substance of the second four weeks was nearly identical, my experience as a physician training in this foreign world was markedly different. By the time I showed up for the second-go-around I was a substantially different physician; it is utterly unconscionable how much things had changed in five months…
how much things had changed in me…
how much things had changed in me as a physician…
how much things had changed in me as a physician responsible for the care of a pregnant woman and her unborn baby…
how much things had changed in me as a physician responsible for the care of a pregnant woman and her unborn baby while being the leader of the medical team.
—–
—–
Suffice it to say, it was an overwhelmingly different four weeks. And by no means was I the lone physician paying excruciating attention to the women and their unborn babies, as I was assisted/supervised by a 2nd or 3rd year OB/Gyn resident and Attending physician, but the knowledge and experience I acquired during the initial four weeks allowed me a level of comfort in my own capabilities that I had not anticipated.
The knowledge and experience in regards to the medical aspects of physiology, biochemistry, and anatomy involved in OB/Gyn were certainly at the forefront of increasing my comfort level, but it was actually my knowledge and experience of the other members of the care team that proved to be my greatest asset.
Not that other medical services in the hospital don’t have exquisitely trained nursing staff, but the OB nurses are in a class all by themselves… and if you don’t respect that, they will bury you. Bury you in a world of cervical checks, bleeding vaginas, and spasming uteri.
Think about that for a second… spasming uteri. It used to give me chills even thinking about it… but that was way back when… when I was still learning about how life sustains us. Now I know to give some gentle uterine fundal massage. And run the pitocin wide open.
—–




2 comments