Allen Street
Author: Dr. Lewis Thomas (1913-1993)
Reprinted from “The Youngest Science: Notes of a Medicine Watcher”
Canto I: Prelude
Oh, Beacon Street is wide and neat, and open to the sky
Commonwealth exudes good health, and never knows a sigh
S collar Square, that lecher’s snare, is noisy but alive
While sin and domesticity are blend on Park Drive
And he who toils on Boylston Street will have another day
To pay his lease and live in peace, along the Riverway
A thoroughfare without a care is Cambridge Avenue,
Where ladies fair let down their hair, for passers-by to view
Some things are done on Huntington, no sailor would deny,
Which can’t be done on battleships, no matter how you try
Oh, many, many roads there are, that leap into the mind
(Like Sumner Tunnel, that monstrous funnel, impossible to find!)
And all are strange to ponder on, and beautiful to know,
And all are filled with living folk, who eat and breathe and grow.
Canto II
But let us speak of Allen Street—that strangest, darkest turn,
Which squats behind a hospital, mysterious and stern.
It lies within a silent place, with open arms it waits
For patients who aren’t leaving through the customary gates.
It concentrates on pending results, and caters to the guest
Who’s battled long with his disease, and come out second-best.
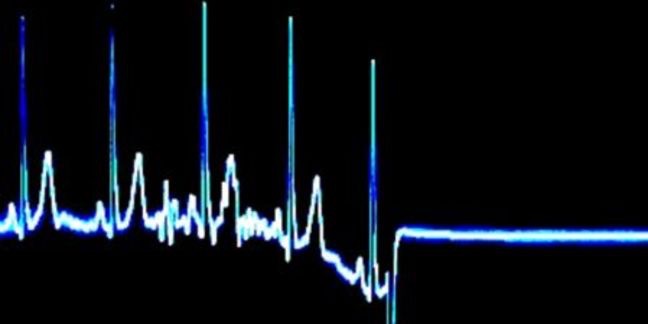
For in a well-run hospital, there’s no such thing as death.
There may be stoppage of the heart, and absence of the breath
But no one dies!
No patient tries this disrespectful feat.
He simply sighs, rolls up his eyes, and goes to Allen Street.
Whatever be his ailment—whate’er his sickness be,
From “Too, too, too much insulin” to “What’s this in his pee?”
From “Gastric growth,” “One lung (or both),” or “Question of Cirrhosis”
To “Exitus undiagnosed,” or “Generalized Necrosis”
He hides his head and leaves his bed, and, covered with a sheet,
He rolls through doors, down corridors, and goes to Allen Street.
And there he’ll find a refuge kind, a quiet sanctuary,
For Allen Street’s that final treat—the local mortuary.
Canto III
Oh, where is Mr. Murphy with his diabetic ulcer,
His orange-red precipitate and coronary?
Well, sir,
He’s gone to Allen Street.
And how is Mr. Gumbo with his touch of acid-fast,
His positive Babinskis, and his dark lunatic past?
And what about that lady who was lying in Bed 3,
Recently subjected to such skillful surgery?
And where are all the patients with the paroxysmal wheezes?
The tarry stools, ascitic pools, the livers like valises?
The jaundiced eyes, the fevered cries, and other nice diseases:
Go! Speak to them in soothing tones. We’ll put them on their feet!
We’ll try some other method, some newer way to treat
We’ll try colloidal manganese, a diathermy seat,
And intravenous buttermilk is very hard to beat
W’ll try a dye, a yellow dye, or different kinds of heat
But get them on their feet
We’ll find some way to treat
I’m very sorry, Doctor, but they’ve gone to Allen Street.
Canto IV
Little Mr. Gricco, lying on Ward E,
Used to have a rectum, just like you or me
Used to have a sphincter, ringed with little piles,
Used to sit at morning stool, face bewreathed with similes,
Used to fold his Transcript, wait in happy hush
For that minor ecstasy, the peristaltic rush…
But in the night, far out of sight, within his rectal stroma,
There grew a little nodule, a nasty carcinoma.
Oh, what lacks Mr. Gricco?—Why looks he incomplete?
What is this aching, yawning void in Mr. Gricco’s seat?
Who made this excavation? Who did this foulest deed?
Who dug this pit in which would fit a small velocipede?
What enterprising surgeon, with sterile spade and trowel,
Has seen some fault and made assault on Mr. Gricco’s bowel?
And what’s this small repulsive hole, which whistles like a flute?
Could this thing be colostomy—this shabby substitute?
Where is this patient’s other half! Where is this patient’s seat!
Why, Doctor, don’t you recollect: It’s gone to Allen Street.
Canto V: Footnote
At certain times one sometimes finds a patient in his bed,
Who limply lies with glassy eyes feeding in his head.
Who doesn’t seem to breathe at all, who doesn’t make a sound,
Whose temperature is seen to fall, whose pulse cannot be found.
And one would say, without delay, that this is a condition
Of general inactivity—a sort of inanition—
A quiet stage, a final page, a dream within the making,
A silence deep, an empty sleep without the fear of waking—
But no one states, or intimates, that maybe he’s expired,
For anyone can plainly see that he is simply tired.
It isn’t wise to analyze, to seek an explanation,
For this is just a new disease, of infinite duration.
But if you look within the book, upon his progress sheet,
You’ll find a sign within a line—“Discharged to Allen Street.”