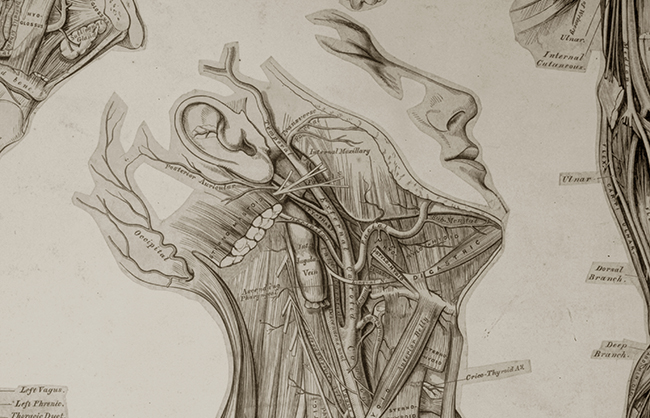
Gray’s Anatomy… continued
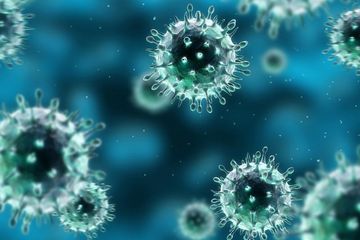
Other than the hub-bub of “gowning up” every time I needed to see a patient, I enjoyed the four weeks I spent on the Infectious Disease service for a few reasons. First off, our Attendings (the most senior physician who bears most of the underlying responsibility) had been stellar, taking the time and effort to teach us what we needed to recognize as physicians to take care of these growing humans.
Secondly, I enjoyed the day-to-day interaction with the 3rd year medical students who were on our service. I could remember being in their shoes only a few years earlier and had been fortunate to have a few interested Residents teach me how to become a physician. So in like mind, I put forth the effort to interject some critical thinking into their minds during rounds and support their own journey towards becoming a physician.
Yet, after a month of slipping into a yellow contact precaution gown and sliding a droplet precaution mask over my face every time I entered a patient’s room, I was elated to transition to the Hospital Pediatrics service, a mini-Clin Med of sorts.
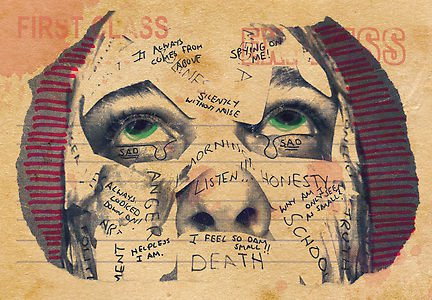
While I was excited to be on this new service, I was shocked to see the amount of behavioral medical issues that came pouring through the ED. Nearly every night, there would be one or two more suicide attempts, psychotic breakdowns, violent traumas, or kids with simply bizarre behavior admitted on to our service.
Even more concerning, was the existence of a second Resident-run Hospital Pediatrics service, who would also “take on” an equal number of similar admissions each night. The number of admissions became so high that at one point a 3rd service was initiated, run solely by Attendings, only for the behavioral medicine admissions.
—–
—–
There is some messed up stuff going on in this world… And one of the points of identification is the Children’s Hospital Emergency Department.
Thankfully, not all is lost and I cared for many children whose medical problems were cured by antibiotics, hydration, technologic advances, and surgical interventions. The look on a parent’s face when their child has survived a hospitalization is incomparable. The intimate relationship you can build over a few hours with another human being when you are their physician, or even more so their child’s, is at the core of why I chose this for my life.
—–
—–
The next stop on the Internship Train was a month of Obstetrics and Gynecology. As I mentioned in Part I, my six weeks of Ob/Gyn as a student resulted in a two-week “Journey to Reclaim My Soul.” So I must admit, I came into the Ob/Gyn service as a resident with a bit of trepidation.
While I was excited to see the first breath of life for many new babies, when you know you are going to be the one sitting on a stool at the end of a bed as a woman pushes that oxygen-requiring baby towards you, there is a bit of responsibility that comes into play. Even armed with the knowledge that women have been delivering babies for centuries upon centuries with minimal medical intervention, when you are the one charged with helping the baby out of the vagina, it seems like the most monumental task in the history of mankind.
I had been allowed to assist in a couple of deliveries as a student, so I could roughly remember the feeling of a slippery newborn, but nothing prepares you (or specifically, me) to show up on Day 1 and deliver a baby.
But that is exactly what I did. And then again. And again. And again.
Each time it happened during the service was similar, but also dissimilar, to the last. My participation seemed to be the least natural thing I could possibly be doing at that given moment in time. Yet, I would go over and over in my head what I was supposed to be doing: where I should be putting my hands on the vagina, how I should cradle the baby’s head as it popped out, where I should clamp on the umbilical cord, who should I hand the baby to, and on, and on, and on.
—–
—-
Until all of a sudden, the baby was resting on the mother’s stomach, I had delivered the placenta, cleaned the “birthing area”, counted the instruments and gauze pads, and was ready to tear off the sterile gown, gloves, face mask, and booties like Walter White leaving the meth lab.
—–
—–
Upon exiting the birthing suite, I would congratulate the mother and surrounding family again, flash a broad smile, and feel the cortisol levels dropping in my blood stream.
A fitting follow-up to Obstetrics and Gynecology was a four-week vacation on our Surgery Out-patient service. Of course, this wasn’t actually a four-week vacation, but when the hours go from roughly 6A-6PM and 6P-6AM to 8a-5p and there are no screaming babies popping out of vaginas, everything seems like a vacation.
Unlike Ob/Gyn where each day was roughly similar in its expectations, this service was filled with a hodge-podge of different surgical specialties. In the Colo-Rectal surgeon’s office I saw more anuses and hemorrhoids than I would care to admit. On Wednesday mornings the Podiatrist would quiz me on foot X-rays and show me how to wield a scalpel on nasty diabetic foot ulcers. The general surgeon had me poking and prodding at inguinal hernias and draining abscesses.
—–
—–
In order to remind us we were not on vacation, but actually real-life-physicians, I also spent a two weekends that month covering the In-Patient surgical service. In effect, it was the Clin Med for Surgeons: replacing electrolytes, ordering pain medications, changing wound dressings, and evaluating patients for surgical emergencies. Not exactly the exciting life of a Trauma surgeon, but I’ve done worse.
My 7th service found me back on… Clin Med. During our Intern year, we spend two months apiece on Clin Med and OB/Gyn, so making it back to Clin Med represented a half-way point in my year… and gave me the feeling I might actually make it after all.